Mother Jen Rowlands began the year with a death sentence. Feeling dizzy, she thought she had sunstroke. Then came seizures, memory loss, leaving her unable to talk or walk. Doctors found five tumours on her brain and more on her lungs.
Rowlands, 43, was shocked to learn she had stage 4 melanoma – which had spread silently since she had a small mole removed from her leg 15 years earlier.
'No-one said to me at the time that melanoma is a really aggressive cancer – there was no education about it back then. Years later, it wasn't even on my mind.”
Heartbroken at the thought of leaving her two young sons without their mother, she collapsed in sobs when doctors told her 'it was advanced – the end of the road”. Surgery wasn't an option, radiation could give her brain damage, and there was nothing that could help.
Unless, as her builder husband Brent says, 'you get your wallet out”.
'We were asked what our budget was, as if we were doing a house. It became clear that money is the difference between life and death.”
An immunotherapy drug could shrink the tumours and extend her life by years, and could even cure her altogether.
The catch? It costs $100,000. The drug, Ipilimumab, is not funded by Pharmac, the Government's medicine buying agency.
The Rowlands don't have $100,000, and their health insurance doesn't cover unfunded medicines.
They've now started private treatment at a cost of more than $5500 a month. It's a lot to fork out as Brian, who has his own business, can't work while looking after Jen.
Results from private treatment readying her for immunotherapy are already 'remarkable”.
From lying in bed constantly fitting, unable to remember her children's names, Jen is up and about, making coffee and laughing with her friend Nicola who'd made a joke that the drug was 'a no-brainer” for the brain tumours.
She's planning to restart yoga and running. She's doing a bit of work from home for the accounting firm she's been with for 19 years.
'The drugs are not just working long term but have given her quality of life back,” says Brent.
'Who would want to die like that, deteriorating and suffering horribly, when there's another option? It feels unfair. We've both worked hard all our lives, paid taxes, ACC, given back to the community, but when it comes to saving a life, there's nothing to help us. Jen deserves a chance.”
Friends started a Givealittle to raise the money. They're organising an auction.
'We are winging it,” says best friend Nicola Gardner, who goes with Rowlands to every appointment, dragging her out of the room where she got her prognosis, telling her,
'Let's get out of this death place, because you're not going to die.”
Under private care, Rowlands has hope, which is helping with healing. She worries about the money even though it's keeping her alive.
'When do you stop?” said Rowlands, no longer laughing, tears pooling in her eyes. 'I don't want Brent and the boys left homeless and poor.”

Jen Rowlands and her friend Nicola Gardner, who goes with her to all the appointments. Photo: Mark Taylor/Stuff.
Immunotherapy is not an obscure pipe dream. Breakthrough immunotherapy drugs like Ipilimumab are viewed as a viable treatment for stage 4 metastatic melanoma, used in combination with other drugs.
A recent study by top melanoma expert Professor Georgina Long, Melanoma Institute Australia, showed melanoma that has spread to the brain responds to Ipilimumab in combination with nivolumbab, and recommends the combination.
Long is about to publish a six-year update, with 'excellent long-term outcomes”.
Ipilimumab has been approved for this use since 2011 by the US regulatory body, the FDA. It's been subsidised in Australia since 2013, when its Pharmaceuticals Benefits Scheme – the Australian version of Pharmac – recognised the 'high clinical need”.
It was funded in the UK in 2016 to treat melanoma in combination with other immunotherapy, with recognition that it could 'significantly improve the life of people.”
Pharmac's director of operations, Lisa Williams, said there would always be more medicines it wants to fund than it can afford, due to a fixed budget set by the government.
Since 2016 Pharmac has funded two immunotherapies, pembrolizumab and nivolumab for treating people with metastatic melanoma stage 3 or 4, who meet specific clinical criteria.
A 2012 application for ipilimumab was initially declined, then Pharmac's clinical advisors revised and said it should be funded, although at 'low priority”. A further application in 2016 was declined.
Professor Chris Jackson, professor of oncology at Otago University said the drug works 'very well” in combination with other immunotherapy drugs.
'It would be an excellent addition to the treatment arsenal for patients with melanoma that has spread to the brain.”
'The notion they fund two immune drugs is disingenuous as they are interchangeable - it's like saying we offer you 91 octane from either BP or Mobil, so we're offering a variety of petrol.”
Pharmac's analysis was done before up-to-date studies, so it is the 'extremely high” cost of ipilimumab that influences Pharmac, he believes.

Professor Chris Jackson, professor of oncology at Otago University said drug companies need to be accountable. Photo: Stuff.
'Too many patients miss out on treatments that could work, or make their lives longer or better.”
Jackson contributed to the recent report by the Te Aho o Te Kahu, the Cancer Control Agency, on the medicines gap in cancer between New Zealand and Australia. It identified four gaps in melanoma treatment – including ipilimumab in combination.
Following the report, and an independent review, Pharmac's funding was increased by $191 million, the largest increase since the agency's inception, boosting its budget to $1.2 billion.
'It was still not enough to fund all the effective cancer drugs that exist, and drug companies need to be held accountable for such extreme prices,” said Jackson.
Melanoma New Zealand chief executive Andrea Newland says funding these lifesaving and life-extending treatments” is vital.
'For too long New Zealand has been winning the race that no-one wants to win … the worst incidence and death rates of melanoma in the world.
'With case numbers projected to increase due to an ageing population and ongoing exposure to high levels of UV radiation, New Zealand can't afford to be complacent.”

Dr Malcolm Mulholland with his late wife Wiki, who died in 2021 from stage 4 breast cancer, after battling Pharmac. Photo: David Unwin/Stuff.
Advance in melanoma treatments in the last 10 years has been 'extraordinary”, she said.
'Ipilimumab is one example of several drugs that are not funded in New Zealand, all of which have the potential to provide very meaningful benefits to patients, such as increased life expectancy and improved quality of life.
Despite this, New Zealanders have not been able to benefit from advances to the same extent as many OECD countries, because treatments remain unfunded and financially out of reach, she said.
Chair of advocacy group, Patient Voice Aotearoa, Dr Malcolm Mulholland, said it was 'appalling and despicable” that people like Rowlands were in this situation.
He can relate. He battled for years to get access to the best drugs for his late wife's breast cancer.
'Pharmac treats access to medicine as a luxury, not a right as in other countries. We have to ask the question: what price is a life? People shouldn't have to fundraise on Givealittle to stay alive.”

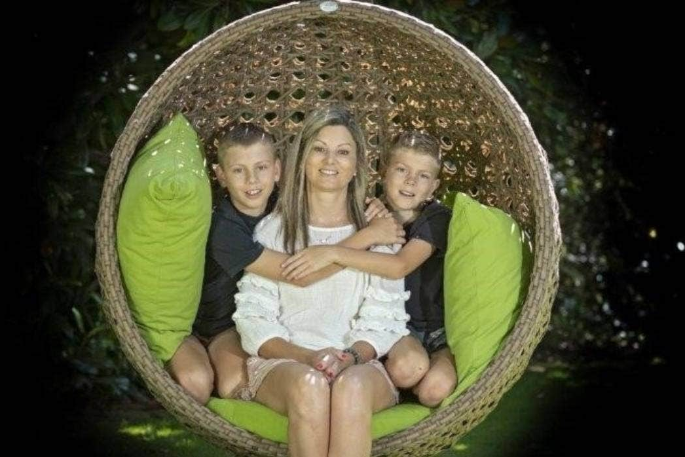
Jen Rowlands wants 'more time” with her young family. Photo: Mark Taylor/Stuff.
Doubling Pharmac's current funding would clear the drugs on its current wish list, but even that would only make New Zealand 'average”.
'Successive governments' underfunding of Pharmac means we're not benefitting from advances in medicine for common diseases, which costs the health system more in the long run.”
For Rowlands, it's a big enough battle to survive.
'We shouldn't have to worry about political issues about medicine that is helping me.”
She calms herself doing puzzles, and smelling the flowers Brent recently planted in their garden.
'I do literally smell the roses a lot,” she laughs.
'I'm grateful that there is treatment that allows me to be healthy enough to be a good mum to the boys, and enjoy life as a family together.”
'I want more time. You shouldn't have to buy that.”
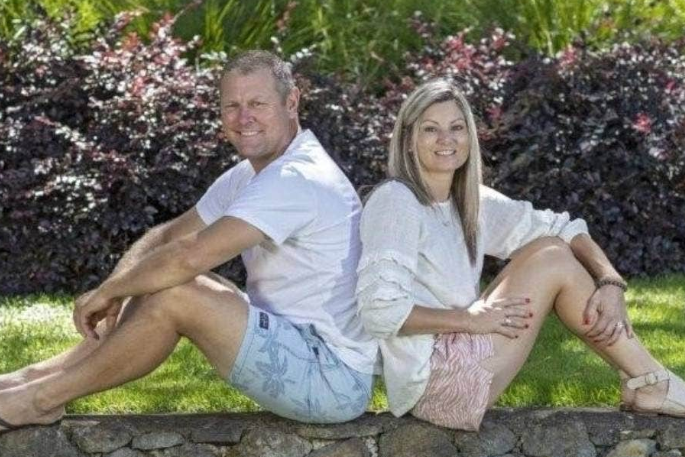
Brent and Jen Rowlands. Photo: Supplied.


2 comments
I feel for Jen.
Posted on 03-03-2023 13:42 | By morepork
She is in a terrible situation and NO kiwi family should have to endure this. I too have melanoma and have been waiting 14 weeks for surgery which is supposed to be "urgent and vital". I've finally taken it into my own hands and had to go private. It is all about money, as the article describes. New Zealand has the highest melanoma rates in the world, and Tauranga is the highest in New Zealand. We are NOT a third world nation and we should be able to do much better than we are. The state of your Bank balance should not decide whether you live or die. When it comes to melanoma... it does. I read the papers on the drugs described and they are very promising. I know Pharmac have to make impossible decisions, but melanoma is a particularly "Kiwi" problem. We should be funding treament.
Treatment
Posted on 03-03-2023 16:54 | By Sycamore2
Unfortunately Pharmac can't fund every medicine.
Leave a Comment
You must be logged in to make a comment.