
Glen Murphy has spent the last six years in a wheelchair paralysed from the neck down.
Despite a judge ruling that his doctor provided him a substandard level of care and should have recognised the symptoms of meningitis he doesn’t receive taxpayer-funded care and has exhausted every appeal, review and legal avenue available to him. Open Justice reporter Jeremy Wilkinson reports.
5.23pm: October 14, 2017.
“He is very agitated,” Glen Murphy’s doctor wrote when he turned up at his clinic, delirious, in pain and coughing up blood.
“In discomfort: muscle spasms, slight tachycardia mild temperature, grinding and chewing motion, distressed and muscle spasms.
“Plan: Norflex to help with the muscle spasms bloods to check his basal functions.
“We will contact tomorrow with results.”
But, tomorrow was too late for Glen who was found unconscious on the floor of his bedroom the following morning.
He was rushed to hospital where he suffered a stroke in his spinal cord. When he woke up from a coma weeks later he found he was paralysed from the neck down.
Since then Glen, who is now 46, has spent more than half a decade bound to a wheelchair as a tetraplegic and has spent most of that time fighting for taxpayer-funded care.
Despite a District Court judge finding that Glen’s doctor should have seen the warning signs of severe meningitis and his treatment was a departure from the standard of care expected from a doctor his claim for cover from the Accident Compensation Corporation has been repeatedly denied.
Now, after more than a six-year fight, Glen has reached the end of his legal road, having exhausted every review and appeal available to him.
“Why won’t they look after me?” Glen has asked himself over and over again.
“Why won’t they help me and my family?”
 Glen Murphy has reached the end of the legal road in his fight for taxpayer-funded care. Photo / Hannah Bartlett.
Glen Murphy has reached the end of the legal road in his fight for taxpayer-funded care. Photo / Hannah Bartlett.
Glen recently sought leave to appeal to overturn a ruling from the District Court declining cover that he hoped would see him receive round-the-clock care, 80 per cent of his wages and a refit of his house to accommodate the wheelchair he will now spend the rest of his life in.
Instead, he receives limited care provided through his local District Health Board which funds carers to help get him up in the morning, feed him lunch and put him to bed.
It’s family who pick up the slack for the rest of his care and they’ve recently started a Givealittle page to take the edge off and give them some respite.
“I feel cheated,” he told NZME from his home in Tauranga.
“I suppose I’m not angry with them [ACC] at the end of the day, I’m just disappointed and upset.”
Legally, it all boils down to one key point; no one can prove that sending him to hospital sooner would have made a difference.
In Glen’s opinion, no one can prove it wouldn’t have made a difference either.
Golden Hour
Meningitis is a bacterial infection that is an inflammation of the meninges - the membrane lining the brain and spinal cord. It is life-threatening and can cause death within hours.
Some of the bacteria that cause meningitis can also cause septicaemia, which is a blood infection that can cause damage to blood vessels and organs throughout the body.
Some people develop meningitis or septicaemia. Other people develop both meningitis and septicaemia at the same time.
There are many types of meningitis including pneumococcal meningitis and meningococcal meningitis. Whilst the symptoms are similar for each, the causes, treatments and outcomes do vary.
The virus itself is incredibly hard to pinpoint because its symptoms are so similar to the drastically more common cases of cold and flu that doctors see every day.
According to data from The Institute of Environmental Science and Research cases of the virus are down from 72 in 2022 to 59 in 2023, and lower than a spike that occurred in 2019 when 139 people were infected with it.
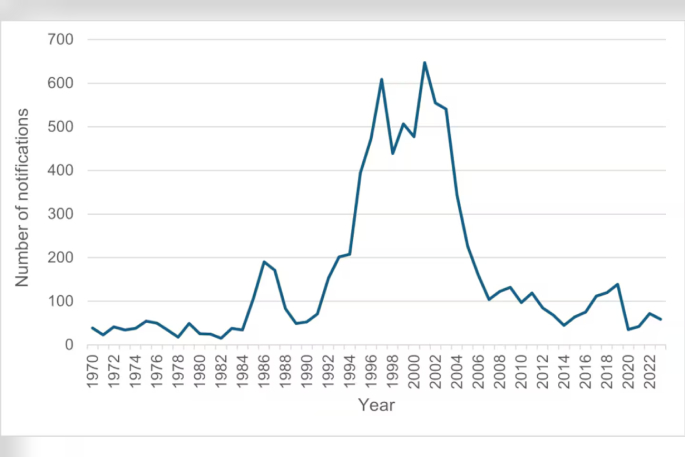 Notified cases of meningococcal disease, 1970–2023. Photo / Te Whatu Ora.
Notified cases of meningococcal disease, 1970–2023. Photo / Te Whatu Ora.
While the numbers of the infection are low the morbidity rate is extremely high. Roughly 20 per cent of those who get it will die and 40 per cent of survivors will have to endure a lifelong disability; deafness, blindness, organ failure, amputation, depression. The list goes on.
It started with a fall from a ladder
In August 2017 Glen fell off a ladder and badly cut one of his hands which became severely infected over the next two weeks and he turned up to his doctor on three occasions with pain in his groin and trouble breathing.
Come Black Friday in October two months later he turned up at the Tauranga Hospital Emergency Department but there are no notes available from his visit.
The next day he turned up at the Waikato Hospital Emergency Department in a delirious state but left before a doctor could see him. That evening he went to his local doctor in distress, grinding his jaw, coughing up blood and having muscle spasms. His GP ordered blood tests and sent him home with a prescription for muscle relaxants.
The next morning his uncle found him unconscious on the floor of his bedroom and he was rushed to hospital where he was found to have a severe case of blood poisoning, or meningitis.
While in the hospital he suffered a spinal cord stroke and was in a coma for five weeks.
When he woke up he found he was paralysed from the neck down. He has minimal use of one hand but it causes him extreme pain.
However, contracting the disease and suffering an injury from it isn’t enough to qualify someone for ACC-funded cover.
 Glen Murphy on his wedding day. Photo / Supplied.
Glen Murphy on his wedding day. Photo / Supplied.
Treatment Injury
In order to qualify for taxpayer-funded care a medical professional has to have made some kind of error in a patient’s treatment that has essentially caused a person’s meningitis-induced disability.
This is known as a “treatment injury” and is the aspect of the legislation Glen's legal team honed in on.
Neurologist Dr David Bourke gave evidence in Glen’s challenge to the District Court in Wellington last year that even a 30-minute delay in meningitis diagnosis is dangerous.
He described a “golden hour” for treatment of the disease which he claims Glen’s doctor missed. If he hadn’t David claims the spinal stroke which caused Glen’s tetraplegia is unlikely to have occurred.
“It is a real pity that this opportunity was missed, as this was likely early in the course of his bacterial meningitis and treatment here would have prevented the infection progressing further,” his evidence to the court reads.
David says in evidence that the signs of meningitis were taught to trainee doctors and a general practitioner should be expected to be able to identify them.
“Early symptoms are hard to pick clinically, but once a patient develops fever and neck stiffness, it should be obvious what needs to happen,” he says.
“There is no other option but to send them to hospital.”
An infectious disease specialist who reviewed the case file in 2018 says in their opinion Glen’s condition fitted someone who had severe sepsis and that there was a reasonable chance that his injury could have been less severe if antibiotics had been started earlier.
Two other GPs echoed that opinion and says they believed the delay in treatment worsened his outcome.
A fourth GP noted that Glen was “almost certainly seriously unwell” and in his opinion, his doctor should have conducted a more thorough history and clinical examination and documented his findings.
A second infectious disease specialist agreed, saying in their opinion Glen’s doctor should have asked more questions or at least scheduled urgent blood tests.
However, he acknowledged it was difficult and somewhat inappropriate as an infectious disease specialist “to judge the standard of care of a GP” and that in the circumstances it wasn’t unreasonable to have made the decision to send Glen home.
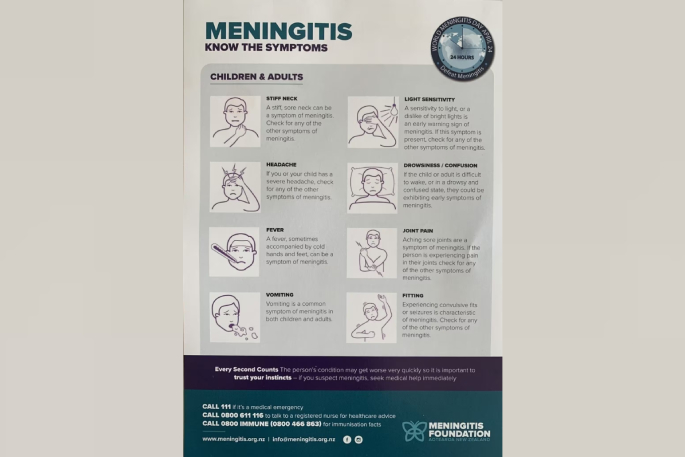 The symptoms of meningitis. Photo / Supplied.
The symptoms of meningitis. Photo / Supplied.
His opinion was that it was unlikely that an urgent referral to hospital and antibiotics would have prevented Glen’s spinal cord injury.
ACC submitted evidence from another GP who also concluded that in his view the notes Glen’s doctor took were of poor quality but was otherwise sympathetic to how difficult to diagnose symptoms of meningitis are.
“… that some of my colleagues have taken some fairly generic physical symptoms from the puzzle and because they know the answer have seen how these pieces fitted into the final picture,” the doctor says in his evidence to the court.
He says that Glen’s doctor was essentially “flying blind”.
“In this regard — he had some generic pieces of the puzzle, but nobody had shown him what the overall picture should look like.”
Glen’s doctor, whom NZME has opted not to name, says in a statement sent by his lawyer that he was unaware of Glen’s fight for cover until contacted for comment.
“The judgments regarding ACC cover do not provide all background facts to the matter, and they evidence the less than straightforward and conflicting views on presentation and care.”
Hail Mary
Glen's claim for cover under a treatment injury was bounced around the corridors at ACC for several years since a doctor at the Burwood Spinal Unit first lodged it on his behalf in 2018.
Following advice from two specialists ACC declined the claim before, in June 2019, a reviewer directed it to investigate further whether Glen’s doctor’s failure to diagnose his meningitis symptoms constituted a treatment injury, and if he had would it have made a difference in the end.
In September 2019 the Corporation’s Complex Claims Panel convened to consider his case before ultimately declining Glen's claim again.
By 2023 Glen’s family had engaged top health lawyer Jonathan Miller to take it to the District Court in Wellington and plead his case before Judge Denese Henare.
Judge Henare found that Glen’s doctor failed to conduct a proper assessment and make a functional enquiry into the symptoms.
“I am satisfied the weight of the evidence shows the flaws in the patient notes reflect the flaws in [the doctor’s] treatment which is a departure from a standard and in consequence, a treatment failure,” her ruling reads.
“[The doctor] failed to conduct a proper assessment, failed to record any attempted history and failed to make functional enquiry especially any negative findings on functional enquiry and these steps could and should have been done, without the benefit of hindsight.”
Judge Henare found that the combination of those failures represented a departure from the standard of care and showed that Glen’s doctor did not have a robust basis to not refer his patient to hospital.
 Glen Murphy and his father Kerry Murphy. Photo / Hannah Bartlett.
Glen Murphy and his father Kerry Murphy. Photo / Hannah Bartlett.
However, Judge Henare found that although there was a treatment failure the court wasn’t satisfied that it caused the injury.
“Even if Mr Murphy should have been transferred to hospital on 14 October 2017, there is insufficient evidence to conclude it is more likely than not that treatment provided 19/20 hours earlier would have materially altered the outcome for him,” she says.
In a last-ditch attempt, Glen then sought leave to appeal the ruling to the High Court.
That attempt was shot down by Judge Peter Spiller in April when he rejected Glen’s bid and upheld Judge Henare’s decision to decline cover.
Vaccination
Meningitis Foundation president Gerard Rushton says Glen’s case is a sad one and an example of why he thinks meningitis survivors should receive ACC-funded care.
“At the moment there’s a gap in the support network for survivors,” he says.
“What really rips my nightie, so to speak, is that if I went out tomorrow and did a ram raid and lost my leg I’d get the latest ‘Blade Runner’ prosthetic, but if I lost it to meningitis I’d get stuff all.”
For Rushton, advocating for awareness about the disease is personal.
He lost his daughter Courtenay in 2016 - they’d been to the doctor three times in two days and it hadn’t been picked up.

“The doctor didn’t go to work that day to kill anyone…meningitis is the worst for a medical professional because it is so hard to diagnose,” he says.
“Our catchphrase here is that every second counts.
“The sooner you get treatment the better your outcome is likely to be.”
The second best way to tackle it is prevention, something the Meningitis Foundation lobbied hard for in recent years before Pharmac announced in 2022 that it would expand its vaccination programme to include children up to one year old as well as 13 to 25-year-olds living in close living situations like in university halls of residence.
According to vaccination data from the Ministry of Health, prior to the rollout at the start of last year less than 500 children under 12 months had received the meningococcal B vaccine from September 2022 through to March 2023.
From March through to August that number had increased 1111 per cent to 51,376.
In the same period, the number of 1-5 year olds receiving the vaccine increased from just 912 to 122,050 while 13 to 25 year olds increased from 808 to 9612.
Across the board that’s more than an 8000 per cent uptick in vaccinations against the virus in the space of six months.
For Rushton, it’s a matter of simple mathematics.
“Compare that to the millions it costs to care for one single person who is disabled because of meningitis for the rest of their life.”
ACC’s Deputy Chief Executive Service Delivery, Amanda Malu, says in a statement to NZME that the decision to decline cover for Glen was based on expert medical opinion that was upheld in the district court.
“In Glen’s case, we found that his meningitis infection was already well-advanced when he attended A&E and that treatment (even if provided 19 hours sooner) would not have had a material impact on the progression of the infection and the injuries he suffered as a result,” she says.
“We truly sympathise with Glen and his family for what they have been through and the ongoing impact to their lives following his meningitis infection.”
Malu says she couldn’t estimate exactly what Glen would have been entitled to if he had been granted cover but did confirm the corporation had spent $31,000 in legal fees challenging his claim through the courts.
ACC Minister Matt Doocey says he couldn’t comment on Glen’s specific case but was aware that Pharmac was looking at expanding access to the meningococcal B and meningococcal ACWY vaccines.
Doocey says that Pharmac currently has four applications in for funding for various catch-up programmes of the various vaccines that are yet to be approved.
Glen wouldn’t have qualified for a dose of the vaccine under any existing or proposed catch-up programme regardless.
And now, without cover and any further legal recourse, he’s completely reliant on the limited care he does receive as well as help from his family.
“We’ve been battling here,” he says.
“My dad has been doing a lot of the work behind the scenes…and it’s been tough on him.”
Otherwise, it’s his wife who looks after him on top of working full time and looking after their two sons.
Glen, who used to be a fitter welder and owns his own business, says now there’s not much he can do except watch television or take his power chair for a drive around the block.
The stroke means he couldn’t play with his kids who were still young at the time of his stroke.
“I’ve just missed so much time with them.”




0 comments
Leave a Comment
You must be logged in to make a comment.